How do I get an at-home COVID-19 test for free?
If you have pharmacy coverage as part of your Health Net plan, you can get an over the counter (OTC), FDA-approved, EUA at-home COVID-19 test at no cost if you visit one of Health Net’s in-network retail pharmacies. View approved in-network pharmacy test kit list (PDF).
Get the test from the pharmacy itself. Do not get a test and pay for it at the store’s normal register. If you pay for the test at the normal register, then you will need to submit a medical claim form to get reimbursed.
Visit our website to find an in-network pharmacy for your plan type.
Are there tests not covered through pharmacy?
COVID test kits that are not covered include:
- Kits that have to be sent to a lab (collection kits)
- Kits that are not indicated as "OTC"
- COVID kits obtained outside of the United States
I have a Health Net group medical plan, but the prescription coverage is through another company. How do I get an at-home COVID test for free?
Check with your pharmacy to see if they can bill the vendor through their pharmacy system. You can then get an OTC at-home COVID-19 test at no cost. You can also purchase an OTC FDA- approved, EUA at-home COVID-19 test and be reimbursed by Health Net for the cost of the test. Please complete and submit a Health Net medical claim form.
I bought an at-home COVID-19 test on my own, will I be reimbursed?
Yes. If you bought an OTC FDA-approved, EUA at-home COVID-19 test at any place outside of our in-network pharmacies (e.g., Amazon, grocery store, drug store, etc.), you will be reimbursed for the cost of the test kits (up to $12 per test) as follows:
- The name of the OTC COVID Test Kit.
- The UPC code found on the box.
- Complete Section 1 and Section 2 of the claim form
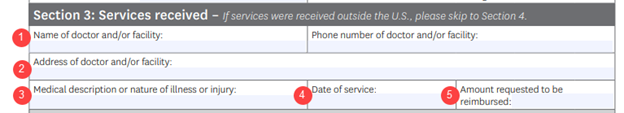
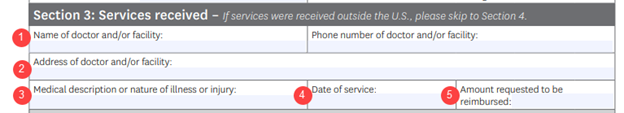
For Section 3, include this information in the fields as follows:
1. The store where you bought the test kit (Amazon, grocery store name, drug store name, etc.)
2. The address of the store if applicable.
3. Write "COVID-19 Home Test" and the number of tests.
4. The date you purchased the kit(s).
5. The amount being asked for reimbursement.
- Sign and return your claim form (don't forget the receipt).
Mail to:
Health Net, LLC
Commercial Claims
PO Box 9040
Farmington, MO 63640-9040
You will be reimbursed based on federal guidance set on January 10, 2022, which states:
- The cost of the at-home test – up to $12 per test
- Maximum of 8 tests per covered member in a 30-day period
- A single testing kit box that includes two tests would count as two (e.g. $12 x 2 = $24)
If you purchased a physician ordered, FDA/EUA approved test before January 15, 2022, Health Net will reimburse the member when the claim form is turned in based on what you paid.
If I bought an FDA-approved EUA at-home COVID-19 test on Amazon, how do I show my proof of purchase?
Please print an image of the digital receipt and submit it along with the claim form. If you can’t provide a digital receipt, please put the order or invoice number for the purchase on the claim form. This is for proof of purchase and tracking. See above FAQ on how to be reimbursed.
Will Health Net limit the number of tests that a member can get for free?
Yes. Health Net will cover 8 OTC FDA-approved, EUA at-home COVID-19 tests purchased over-the-counter per covered member in a 30-day period. This follows the federal guidance released on January 10, 2022.